(Editor's Note: On March 16, 2020, Gov. Tom Wolf ordered a statewide shutdown in response to the emerging coronavirus threat. This article is part of a series marking the second anniversary of the pandemic in Lancaster County.)
"I was sort of thrust into this position," Dr. Michael Ripchinski said.
Two years ago in mid-March, he recalls, he was asked to take part in a press conference about an emerging public health threat: A deadly coronavirus that was spreading worldwide from its origin in the Wuhan region of China.
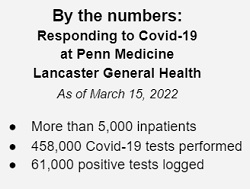
 That media appearance led to another, and then another. Today, Ripchinski, the chief clinical officer at Penn Medicine Lancaster General Health, has become perhaps the most visible and recognizable spokesperson for the Lancaster region's Covid-19 pandemic response.
That media appearance led to another, and then another. Today, Ripchinski, the chief clinical officer at Penn Medicine Lancaster General Health, has become perhaps the most visible and recognizable spokesperson for the Lancaster region's Covid-19 pandemic response.
He has played a key role behind the scenes as well, working with other health systems and stakeholders to coordinate resources and serving as director of the mass vaccination site that operated at Park City Center last year.
Over the winter, the omicron variant of pushed Lancaster County's Covid-19 case counts and inpatient counts to record levels. Since surge has been followed by an equally dramatic decline, raising hopes that after two years, life can return to something approaching normal.
One United Lancaster spoke with Ripchinski about the second year of the pandemic, and what the coming months may bring. The following has been edited for clarity and length.
One United Lancaster: The last time I heard you speak at length about Covid, it was mid-January. We were in the upsurge of omicron. I know we had at one point more than 230 patients countywide.
Ripchinski: There were 152 [LGH Covid-19 inpatients] on Jan. 10. We're under 10 now. So, it's been pretty remarkable to see, in two months, such an incredibly steep drop-off. ...

There are probably many reasons why we saw such a steep decline in cases. Most notably, we had higher vaccination rates than we did last January. So that's good news.
I think it's coupled with the fact that omicron was so much more transmissible than delta. So that makes it natural immunity plus the base vaccination rate. I think we got to a point where the virus burnt itself out, if you will. Cases went down, and so did hospitalizations and deaths.
OUL: What do we know about the seasonality of Covid?
Ripchinski: When you look back at our inpatient census from last year, we hit our nadir around March 8. But then we went from 20 to 80 admissions by April 21. Given how transmissible omicron was, and the vaccination rate, I'm hopefully optimistic that we're not going to have another mini-surge in late April, like we did last year. But that's unknown at this point.
I think signs are more positive than last year that we can get through the spring and summer. The epidemiologists are saying this is probably going to be a winter virus and a need for boosters may occur. We'll see how our risk reemerges, potentially, in the fall.
The reason we're all hedging on this (is that) vaccination rates across the world are still not that great. You may have another country where a potential variant emerges because of low vaccination rates or low natural immunity. Where does that variant travel? How easily can it travel across the globe?
OUL: Were there local blood shortages, and how were they dealt with?
Ripchinski: We certainly had local blood shortages, as all the health systems faced. Being a Level One trauma center makes us particularly acutely aware of that, being a large cancer institute.
Given that high daily use of blood, it certainly made us nervous during the during the last surge, but luckily, and thankfully, we had over 1,000 employees donate in the last four to six weeks — an incredible outpouring from our community and our employees to help us rebuild the blood supply.
OUL: Over the past year, we saw vaccination and boosting; and the development of additional effective treatments. I was wondering if we could address each of those in turn. So, first, what's the state of play with vaccination?
Ripchinski: Let me go back to your (previous) question, because (there's) something I didn't think of ... I mentioned the vaccines and natural immunity, but I should have added monoclonal antibody treatments and availability of oral medication. Granted, those are limited, but they treated several hundred patients who (otherwise) probably would have ended up in the hospital.
So, back to your question. We certainly have an incredible availability of vaccine, more than ever before. We certainly have an incredible amount of safety data. I would venture to say we have more safety on the mRNA vaccines than any other vaccine in the last decade.
And the oral medications are more widely available now, right? The supply has been increasing, but the case load has been going down. So, it really positions us well to create a stockpile, so if we have to use those medications into the fall season, when Covid may potentially increase before people get their boosters, it's going to enable us to have more effective treatments for the next surge.
OUL: Are there any more treatments coming down the pipeline?
Ripchinski; I don't know if there are any new oral medications that I have seen yet that are close enough to talk about. There are many trials, many vaccine trials. There are hundreds of trials going on. The question is, how far along are they? Are they going to get approved? What's their efficacy going to be?
If I was going to summarize: They well position us for the fall. We're going to have vaccines, we're going to have monoclonal antibodies, we're going to have oral treatments. We're going to be in a much better position to, hopefully, quell any future surge.
OUL: About the test center at the Public Safety Training Center, I got the impression it was needed for maybe two weeks and then it kind of tailed off.
Ripchinski: Like any surge, we couldn't appreciate how long (omicron) was going to be, how high it was going to go. (It's) a real credit to the team for putting that together so quickly and getting it stood up with the county. As a result, 2,500 people didn't need to have an urgent care visit, to get a test. They didn't need to go to our primary care practices. So we created capacity where there wasn't, quickly.
OUL: Let's imagine we get to October and numbers start ticking up. What do you anticipate happening? Might there be a mask recommendation that goes out?
Ripchinski: I think so. I actually like the way the CDC is — you know, people give the CDC a hard time about changing. But as a scientist, I recognize that if we're not changing, we're not learning. And I appreciate the fact that they took in new information and they made new guidelines. I don't think there's anything wrong with that. ...
(The CDC's new guidelines on Covid-19 risk levels incorporate new cases, hospital admissions, and the portion of hospital beds occupied by Covid-19 patients.)
Lancaster County has incredible hospital capacity. It's soon to have more. So, the ability to have enough beds to treat our population if they need hospital care is a really good thing. And using that as a factor in the decision making for masking is also a smart thing. And I think that logic probably will apply to future surges. What's the capacity in the ICU, what's the capacity of hospital beds?
But it's not just available beds. This is where I struggle, because we saw it during the latest surge and the previous surges: How many people put off cancer treatment, heart failure treatment, didn't come to the hospital, because they're worried about getting Covid? That treatment delay aspect really bothers me. We may have enough beds to take care of all the Covid patients that come in, but who withholds or stops or prevents or delays treatment?
OUL: To that point, where do things stand on staffing? There's been a lot of concern about frontline health care workers.
Ripchinski: Tiredness, fatigue, burnout, are all current factors for our staff. There's a sense of relief, given where we are currently. But, you know, two weeks of relief doesn't remove two years of burnout. That is a concern of mine and a concern of the entire executive and leadership team. We're trying to work with the staff to figure out new ways to think about work and ways to improve our work processes.
OUL: On long Covid, what are you seeing? What concerns might you have?
Ripchinski: We certainly are seeing long Covid, and more science is coming out regarding potential causes. We need more studies on why certain people are potentially experiencing more long-term symptoms.
If they are, the advice I would give is to seek out a post-Covid clinic. We have post-Covid syndrome clinics here at LGH in connection with Penn Medicine. If you're experiencing long term fatigue, shortness of breath, heart palpitations, we want to see you.
OUL: Any other takeaways you would like the public to hear?
Ripchinski: I really appreciate the community's support of our health care teams. It's been an incredibly challenging few years, so I want to thank them for that.