For the past year, elderly residents in nursing homes have suffered most from the COVID-19 pandemic.
The lopsided death toll is difficult to comprehend: Of the 974 county residents killed by the virus, 95% have been age 60 and older. Half have lived in nursing homes.
The arrival of vaccines is fast changing all that. With mass inoculation of nursing home residents and staff, as well as the general population over age 65, COVID-related hospital cases and deaths are in steep decline.
• The average number of COVID patients at Penn Health Lancaster General and WellSpan Ephrata daily has plummeted 70% – from 115 in January to 32 in March.
• Deaths have fallen even more, down 80%, from five per day in January to less than 1 per day in March.
As positive as those trends are, the suffering that the elderly endured in nursing homes and the lessons learned by the staff and administrators there should not be pushed out of mind, like some hideous nightmare, in the eagerness to resume normal, pre-pandemic living.
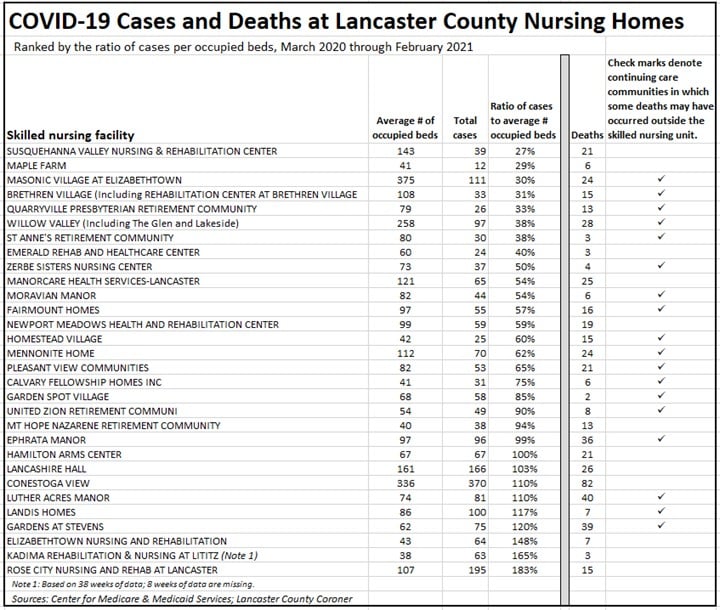
For that reason – to begin the process of documenting what happened in nursing homes here – retired sociology professor Dr. Mary Glazier has compiled comprehensive data on reported cases of COVID-19 at all Lancaster County nursing homes.
She has matched that information with the average number of occupied beds at each facility to provide a ratio that shows the extent to which homes were able to control the virus among their residents.
Her data rank the nursing homes of Lancaster County from those with the lowest infection rates to those with the highest, the first time that has been done here.
How the data was compiled
Dr. Glazier obtained the total case numbers and occupied bed counts for each facility from the Centers for Medicare and Medicaid Services, which, unlike the state Health Department, has been able to receive and publish complete data from the homes throughout the pandemic. She obtained the information on deaths from the Lancaster County Coroner’s Office.
Because the number of residents (occupied beds in government records) varies from week to week, this study used an average of weekly numbers to provide an estimate of occupancy throughout the past year.
In some facilities, there is a seeming oddity – the number of COVID cases exceeds the number of residents. This situation occurs because most homes have a steady turnover of residents. Some recover from illness and move to a non-nursing unit. Some transfer to another home. Some die.
It is essential for the reader to recognize that this information is a starting point for research, not an end point. It should not be used to evaluate the relative performance of nursing homes.
Why? Because many factors influence the rate of infection and deaths. Among them:
• Timing. If the virus hit a nursing home early in the pandemic, before protective equipment was available and before the best practices and treatments were established, it may have a high percentage of infections.
• Pre-pandemic health of residents. Some facilities may have had a higher number of severely ill residents, more susceptible to the virus, than other facilities had at the outset of the pandemic.
• Staff expertise. Some homes may have had more registered nurses, able to supervise aides, than did others.
• Location. To the extent that staff may bring the virus into a home, the community where the staff live may have influenced the rate of infection.
We are publishing this data in the hope that others will use it, and similar data from other communities, to learn what factors actually increased or decreased the spread of COVID-19 within facilities.
With those limitations in mind, the five homes with the lowest percentage of cases were Susquehanna Valley Nursing & Rehabilitation Center, Maple Farm, Masonic Village, Brethren Village, and the Quarryville Presbyterian Retirement Community.
The five homes with the highest percentage of cases were Rose City Nursing and Rehabilitation, Kadima Rehabilitation & Nursing, Elizabethtown Nursing & Rehabilitation, The Garden at Stevens, and Landis Homes.
The range of infection rates is immense. The highest rate (183%) is nearly seven times larger than the lowest rate (27%).
Now, as the pandemic recedes, particularly in nursing homes, while data and memories are fresh, researchers have their best opportunity to learn the reasons.